How to Make AI and ML-Based Medical Image Analysis Better.
Medical images such as computed tomography (CT), magnetic resonance imaging (MRI), mammograms, X-Ray types such as fluoroscopy and angiography, and ultrasounds are a valuable trove of potentially life-saving data for healthcare researchers, providers, and their patients.
But these kinds of images also present unique challenges that have traditionally limited radiologists’ effectiveness in diagnosing and treating various ailments. Consider that most medical image analysis today is performed by only a small group of (often overworked) radiologists or clinical doctors. That means the interpretations of these scans are, at best, extremely subjective – and, at worst, they can be entirely off base.
Indeed, medical experts say one in four patients experience false positives from their medical image review, thanks to such challenges as reviewer fatigue and the increasing complexity of the images themselves. And while false positives are slightly better than false negatives – which can lead to a potentially fatal condition going untreated – they’re certainly not fun, as they can lead to unnecessary follow-ups or even surgery (along with unnecessary stress to the patient, and costs to the health system).
The promise of AI for scanning medical images
Traditional manual medical image review processes have saved countless lives over the years – but that doesn’t mean these processes can’t be improved. Indeed, machine learning (ML) technology can analyze and learn from vast quantities of data, while performing computer vision (CV) analysis on an image to find minute differences the human eye can’t catch – are already showing enormous promise. Along with deep learning (DL), a form of machine learning based on artificial neural networks, these technologies have made automated, accurate, and ultra-fast medical image analysis a reality.
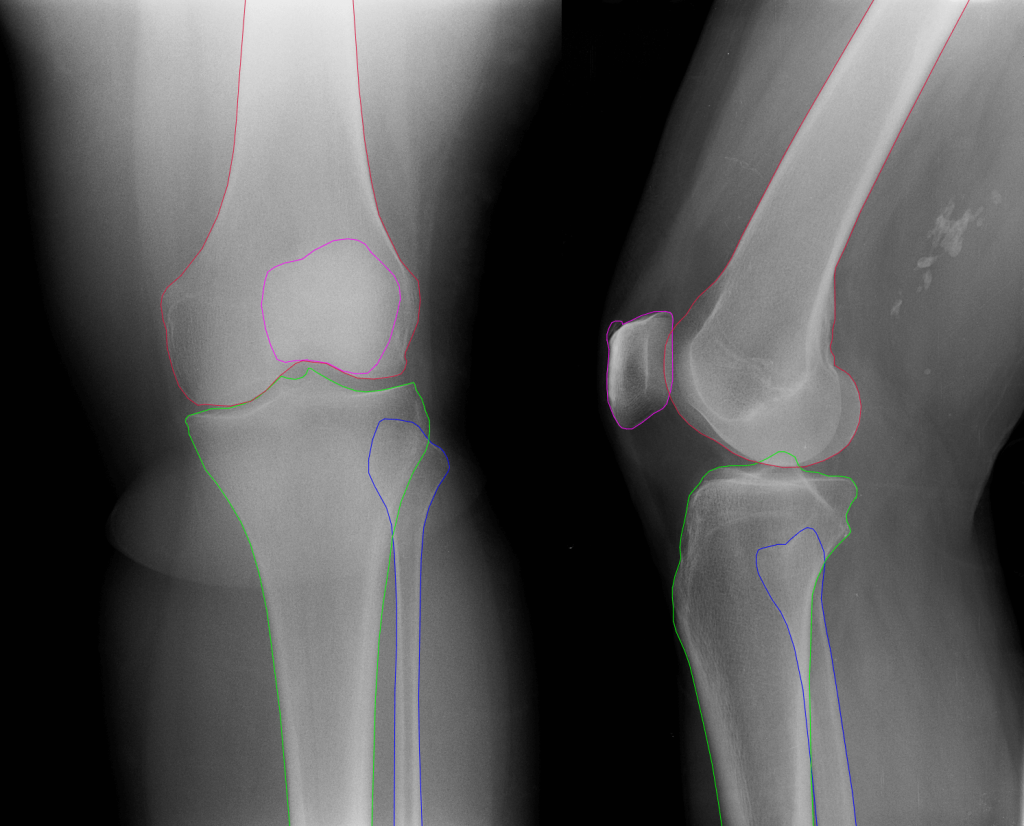
According to medical and technology researchers, ML and DL can achieve high performance when analyzing medical images “for detection, segmentation, classification, and prediction”. The researchers say that image scanning using AI algorithms accomplishes better results by involving a multidisciplinary team clinical, imaging, and technical expertise in developing them. “Several tasks traditionally performed by radiologists such as lesion detection, segmentation, classification, and monitoring may be automated using deep learning techniques,” the researchers write.
Along with the apparent function of diagnostics, researchers say AI can also play a role in determining which imaging procedure and (if necessary) treatment selection strategy makes the most sense based on the patient’s condition, their medical records, and potential allergies, and other data. These same researchers say AI can be used to determine how to administer contrast before an examination, and to improve how medical images display within picture archiving and communication systems (PACS). “DL could help automatically arrange image display by using previous patterns and identifying image series that is likely to be useful, based on preferences,” they say, adding that other researchers are experimenting with AI systems based on “deep convolutional neural networks (CNNs), for automated real-time triaging of adult chest radiographs.”
In the UK, these researchers say, these systems have helped shrink the average reporting time for critical imaging findings from 11.2 to 2.7 days – a significant (and possibly life-saving) difference.
AI and ML provide several well-documented benefits for radiologists and clinicians looking to improve and speed up medical image analysis outcomes, including:
- Speed and consistency: AI can assess a massive number of variables faster and more consistently, and can automate workflows to ensure time-sensitive cases get seen first.
- Radiologist support: AI can automate everyday tasks, eliminating human error, and freeing up radiologists for more important things such as complex research or interacting with patients. It can also help aid decision-making and improve diagnostic accuracy and can aid image analysis in other ways through pattern recognition and classification.
- Improved objectivity: Because humans are subjective animals with varying degrees of capability, the quantitative and objective nature of AI algorithms can help remove natural cognitive bias, prejudice, and presuppositions from clinical diagnoses.
The challenges of AI and medical image analysis
But just because AI shows excellent promise doesn’t mean it’s an automatic panacea, either. Training is one issue. ML models’ performance depends on the quality of the training data. Training ML models for accuracy is standard procedure, but can be particularly onerous for medical imaging applications since they often require substantial amounts of accurately-labeled and annotated data – often more than currently available. “Labelling large datasets for training high-capacity neural networks is a major obstacle to the development of deep learning-based medical imaging applications,” argues DA Wood et al.
“Unlike traditional computer vision tasks where image annotation is simple (e.g., labeling dog, cat, bird, etc.) and solutions exist for large-scale labeling… assigning radiological labels to magnetic resonance imaging (MRI) scans is a complex process requiring considerable domain knowledge and experience.” CapeStart offers services to annotate and label pharma, dental, ophthalmological, and other medical images such as CT scans, MRIs, X-Rays, mammograms or ultrasounds.
Deploying ML models for clinical use is also challenging because of the nature of clinical situations, where thousands of variables can be at play – unlike even a vast amount of training data. Diagnostic and other healthcare-related ML models can struggle in these situations, outside a controlled environment with only a few variables, and also face challenges in testing and obtaining regulatory approval.
What can AI do for radiology both now and in the future?
It’s unlikely that we’ll see fully AI-driven diagnostics anytime soon. But the technology can still provide a massive help as an assistant to human radiologists, thus improving healthcare outcomes. Indeed, several tasks traditionally performed by radiologists such as detection, segmentation, prediction, classification, quality checks, and monitoring can be partially or even fully automated but supervised with expert human oversight.
Along with helping radiologists automate mundane yet time-consuming tasks, ML models show great promise – and, indeed, have already proven their value – when it comes to improving the speed and quality of medical image and radiology analysis and reporting. Automated tissue density assessments in mammographic images, for example, can help predict which patients may be at the most significant risk – giving them a higher priority and potentially more timely treatment.
Clinicians say ML and DL can help with tracking lesions and tumors once diagnosed, which is often tedious work requiring relentless follow-ups with patients. “Many of our CT scans are on cancer patients we follow up every three months, and we need to track lesions and measure them to adjust their therapies,” says Charles E Kahn, professor and vice chairman of radiology at the University of Pennsylvania, in Healthcare IT News. “Not only is this tedious work, but also a real opportunity to improve all of these measurements with AI.”

